11 Points of Vascular Dementia
Vascular dementia challenges people and their families. It affects cognition and everyday life. Knowing the ins and outs of vascular dementia and how to manage it can help people live with it with grace and resilience. In this step-by-step guide, we’ll explore 11 things you need to know about managing your mind’s resilience with vascular dementia.
Understanding Vascular Dementia
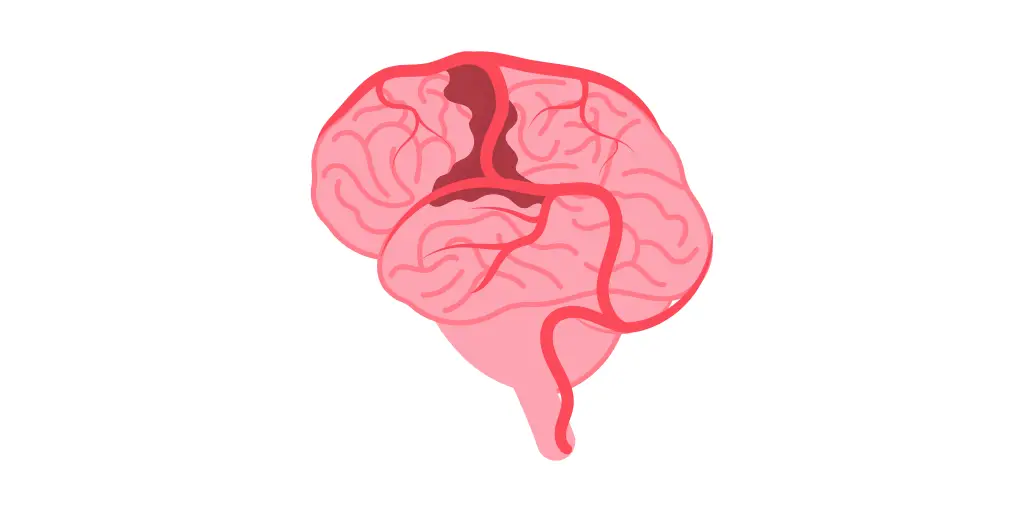
Unlike other forms of dementia, vascular dementia has one thing in common: it’s caused by a blockage in your blood flow to your brain. When your blood flow is impaired, your brain cells don’t have the oxygen and nutrients they need to function properly. It’s like a city whose streets are clogged with traffic, preventing essential goods from getting to where they need to be.
Think of your brain as a busy city. You rely on your blood vessels (roadways) to move oxygen and nutrients around your brain. When these essential pathways are blocked or disrupted, your brain regions experience a shortage of resources. Over time, this can lead to memory loss, thinking problems, personality changes, and other cognitive issues.
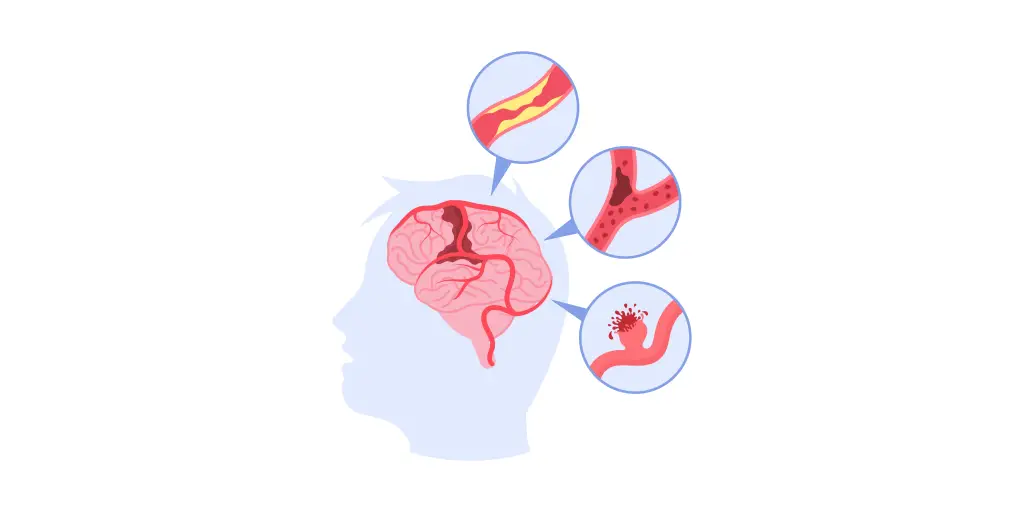
Vascular Insults to the Brain

The main causes of vascular dementia are often caused by vascular damage to the brain. These can be caused by small or large strokes that reduce blood flow to the brain and cause damage to brain tissue. In addition, conditions such as atherosclerosis, in which the arteries become narrowed and hard, and conditions that affect the small blood vessels within the brain can also lead to vascular dementia.
The Cognitive Mosaic of Vascular Dementia
Vascular dementia’s symptoms are like chameleons, changing depending on the affected area of the brain. Memory loss, difficulty thinking, loss of planning and organization, mood swings, changes in personality, and loss of language skills are common symptoms. However, the hallmark of this condition is the unpredictable onset and progression of symptoms, from slow decline to sudden changes, which reflect underlying vascular events that disrupt blood flow.
Managing the underlying risk factors for vascular dementia is important. However, mentally stimulating activities such as puzzles, play, reading, or social interaction can help to empower individuals. Neuroplasticity is the brain’s natural capacity to adapt and create new neural connections. These activities may help to preserve cognitive function and delay the progression of the disease.
It is important to consult a healthcare professional for diagnosis, tailored treatment plans, and support strategies.
Risk Factors

Know your risk factors
- High blood pressure
- Diabetes
- Unhealthy cholesterol levels
- Smoking
- Existing cardiovascular disease
- Cognitive decline
Here’s the good news: there’s hope!
A healthy lifestyle can help reduce the risk of vascular dementia.
A healthy diet, regular exercise, and good cardiovascular health, combined with appropriate medical management, can help you take control of your health and reduce your risk.
Remember, it’s important to speak with a healthcare professional for personalized advice and strategies to improve your overall health and cognitive function.
Diagnosis Dilemmas

Determining whether or not a person has vascular dementia can be like a detective’s investigation. It starts with understanding the individual’s medical history, followed by a multidisciplinary approach that includes cognitive assessments to measure mental function, neuroimaging tests such as MRI scans to visualize the brain, and, in some cases, laboratory tests to exclude other possible causes. Diagnosis is complicated, but standardized criteria such as the DSM-5 help clinicians understand the differences between vascular dementia and other forms of cognitive impairment, so they can make an accurate diagnosis.
A Spectrum of Vascular Involvement
While some of these subtypes share some common risk factors, such as high blood pressure or diabetes, vascular dementia comes in many forms.
For example, multi-infarct dementia, caused by several small strokes, or strategic dementia, caused by a single stroke in an important brain region. These subtypes emphasize the many ways vascular involvement affects the brain, each of which presents its unique challenges and requires a personalized management approach.
While the common risk factors can be addressed through lifestyle changes and medical management, there is still much work to be done to potentially reduce the risk of vascular dementia and improve overall cognitive health. It’s important to remember that speaking with a healthcare professional is essential for accurate diagnosis, personalized treatment, and support for those living with or at high risk for vascular dementia.
Preventive Strategies

Because vascular health is so closely related to vascular dementia, prevention strategies play an important role.
- Manage risk factors:
- Control high blood pressure and diabetes through lifestyle changes and medications.
- Maintain a healthy lifestyle:
- Engage in regular physical activity.
- Follow a balanced diet rich in fruits, vegetables, whole grains, and lean protein (inspired by the Mediterranean diet).
- Quit smoking.
- Manage stress:
- Implement stress management techniques like meditation, yoga, or spending time in nature.
Treatment Approaches

Vascular dementia is a condition in which the brain’s vascular problems become progressively worse and symptoms become more severe. There’s no cure for this condition, but there are several treatments that can help manage symptoms and manage the underlying vascular problems.
Medications that control risk factors for vascular dementia (such as blood pressure or cholesterol) are commonly prescribed. Medication that improves blood flow and improves cognitive function may also be prescribed. Supportive therapy, such as cognitive rehabilitation and exercise, plays an important role in preserving functional abilities and improving quality of life.
The Role of Caregivers

The best way to support someone with vascular dementia is to be empathetic, patient, and knowledgeable. Caregivers provide emotional support, help with everyday tasks, and create a safe and caring environment.
The best way to navigate this journey is to equip caregivers with knowledge about the condition, how it progresses, and effective communication strategies. This empowers caregivers to develop a compassionate and well-informed approach, which ultimately promotes the well-being for the person with vascular dementia and the caregiver. Don’t forget that support groups and respite care, as well as educational resources, can help reduce caregiver burden and give them the tools they need.
Lifestyle Modifications

The best way to prevent vascular dementia is to live a healthy lifestyle. This includes engaging in regular physical activity, eating a balanced diet that includes plenty of fruits, veggies, whole grains, and lean protein (similar to the Mediterranean diet for heart health), quitting smoking, managing stress, and more. All of these lifestyle changes help to improve your cardiovascular health, which may help lower your risk for vascular dementia and improve your overall brain health. It is important to consult a healthcare professional for personalized advice and strategies to improve your overall health and cognitive function.
Cognitive Changes
Living with vascular dementia comes with its own unique set of challenges, both cognitive and emotional. While engaging in mind-engaging activities such as puzzles and socializing can help keep your brain functioning, the emotional impact cannot be ignored. People with vascular dementia and their families often feel a variety of emotions, including sadness, anger, and fear. Fortunately, taking proactive steps can help you feel more empowered.
Brain-enhancing activities can help slow cognitive decline, and having a support network of loved ones, healthcare professionals, and support groups, as well as mental health resources, can help you navigate the challenges of vascular dementia on many levels. Don’t forget to consult a healthcare professional for personalized strategies and emotional support throughout this journey.
Conclusion
Strengthening your mind’s ability to cope with vascular dementia requires a multi-faceted approach that includes understanding, empowerment, and support. By following the 11 key points in this guide and creating a supportive care environment, people living with vascular dementia can lead their lives with dignity, grace, and resilience.
Also Read: Understanding the Common Cold: Essential Insights and Remedies
Quick Answers
Is vascular dementia reversible?
It is typically not reversible; however, early intervention and effective management strategies can help slow its progression and improve the quality of life for affected individuals.
Can lifestyle changes reduce the risk of vascular?
Yes, adopting a healthy lifestyle that includes regular exercise, a balanced diet, smoking cessation, and stress management can help reduce the risk of vascular dementia by promoting cardiovascular health and preserving cognitive function.
What role do medications play in the treatment of vascular dementia?
Medications may be prescribed to manage underlying vascular risk factors, such as hypertension, diabetes, and high cholesterol. Additionally, medications may be used to alleviate symptoms such as depression, anxiety, and agitation.
Are there clinical trials available for vascular dementia?
Yes, ongoing clinical trials are investigating new therapies and interventions for vascular dementia. Individuals interested in participating in clinical research can consult with their healthcare providers or visit online databases, such as ClinicalTrials.gov, to explore available trials.